By: Kelly Gleason, PhD, RN
If you are diagnosed with atrial fibrillation, you and your provider will calculate your risk for stroke and whether you may benefit from an anticoagulant.
How do health care providers calculate this? They give you a score on a scale of 0 to 9. You have a history of high blood pressure? That’s one point. Your “high blood pressure” could mean an occasional blood pressure reading of 135/86 or consistent blood pressure readings higher than 160/90… but, no matter, you get one points for “a history of high blood pressure.”
You get another point for a history of congestive heart failure. But how severe is your congestive heart failure? What is your ejection fraction? No matter, one point for heart failure. One point if you have diabetes. But do you rarely take medication and control your type 2 diabetes with diet? Or are you dependent on insulin because you have type 1 diabetes? No matter, one point for diabetes.
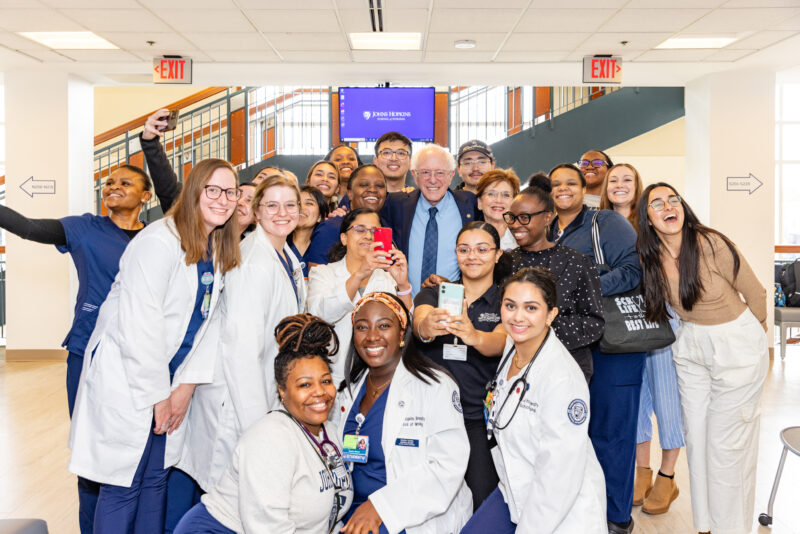
Dr. Harlan Krumholz, an accomplished cardiovascular researcher and physician at Yale, shared this example at Augmenting Clinical Intelligence with Machine Intelligence to Improve Patient Outcomes to demonstrate how far we have to go in medical science. The workshop was hosted on October 12 by the Johns Hopkins School of Nursing and the Whiting School of Engineering. It brought together nurses, physicians, researchers, and computer scientists to take the first step toward building long-lasting, collaborative teams that will improve health outcomes by making patient care smarter.
Today we have an incredible amount of data at our fingertips since more health care providers use electronic medical records and other technologies, and because machine learning only continues to advance. Tools and methods, like those for predicting stroke risk and the need for anticoagulation in patients with atrial fibrillation, can be smarter. Nurses can work with computer scientists to build models that not only account for complexities like severity of hypertension and diabetes, but also to find factors that impact stroke risk that even now we don’t know about.
At Augmenting Clinical Intelligence with Machine Intelligence to Improve Patient Outcomes, the variety of perspectives represented led to some amazing, innovative ideas.
“Is it possible to provide information about palliative care to a person the first time they buy adult diapers for their loved one?” asked Dr. Karl Lorenz, a palliative care physician from Stanford.
Dr. Harlan Krumholz asked, “With a patient’s permission, can we see their grocery store receipts to understand how their diet may impact their health?”
Then, I asked, “If Target can send coupons for diapers to a women who googled symptoms typically associated with pregnancy before she even knows she is pregnant, can we also use this information to connect patients to health care resources?”
Answering these questions requires even more collaboration that adds ethicists and patient advocates to the mix. Ethicists, patient advocates, health care providers, engineers… and, of course, nurses, who are an essential component of these efforts.
Kelly Gleason served as chair of Augmenting Clinical Intelligence with Machine Intelligence to Improve Patient Outcomes. This workshop is only the beginning of nurses, engineers, and allied health professionals collaborating to leverage digital data and machine learning to deliver precise care.
ABOUT THE AUTHOR:
 Dr. Kelly Gleason, Assistant Professor at the School of Nursing, teaches informatics. In her research, she aims to develop methods of reducing diagnostic error through patient-facing health information technology tools.
Dr. Kelly Gleason, Assistant Professor at the School of Nursing, teaches informatics. In her research, she aims to develop methods of reducing diagnostic error through patient-facing health information technology tools.